Abstract
Marinesco–Sjögren syndrome (MSS), first described in 1931, is an autosomal recessive condition characterised by somatic and mental retardation, congenital cataracts and cerebellar ataxia. Progressive myopathy was later reported to be also a cardinal sign of MSS, with myopathic changes on muscle biopsies. Hypergonadotrophic hypogonadism and skeletal deformities related to pronounced hypotonia were also reported. The major differential diagnosis of MSS is the syndrome defined by congenital cataracts, facial dysmorphism and peripheral neuropathy (CCFDN), which is localised to 18qter. Using homozygosity mapping strategy in two large consanguineous families of Turkish and Norwegian origin, respectively, we have identified the MSS locus on chromosome 5q31. LOD score calculation, including the consanguinity loops, gave a maximum value of 2.9 and 5.6 at θ=0 for the Turkish and the Norwegian families, respectively, indicating linkage between the disease and the D5S1995-D5S436 haplotype spanning a 9.3 cM interval. Patients of the two families presented with the strict clinical features of MSS. On the other hand, the study of two smaller French and Italian families, initially diagnosed as presenting an atypical MS syndrome, clearly excluded linkage from both the MSS locus on 5q31 and the CCFDN locus in 18qter. Patients of the two excluded families had all MSS features (but the myopathic changes) plus peripheral neuropathy and optic atrophy, and various combinations of microcornea, hearing impairment, seizures, Type I diabetes, cerebral atrophy and leucoencephalopathy, indicating that only the pure MSS syndrome is a homogeneous genetic entity.
Similar content being viewed by others
Introduction
Marinesco–Sjögren syndrome (MSS) is a recessively inherited disorder first described by Marinesco et al1 in a family of Romanian origin and further characterised by Sjögren2 in families of Swedish origin. Since then, many cases have been reported from various geographic origins. Consistent features of this condition are bilateral cataracts, mild to moderate mental retardation, cerebellar ataxia due to cerebellar hypoplasia, short stature, hypergonadotrophic hypogonadism, and skeletal deformities,3,4 such as kyphoscoliosis, pes planovalgus, short metatarsals and metacarpals, coxa valga, genu and cubitus valgus or pectus deformities. Progressive muscular weakness and muscle atrophy were also reported to be leading features of MSS.5 Myopathic changes including variation in fibre size, proliferation of internal nuclei and rimmed vacuoles were described on most muscular biopsies.5,6,7,8,9,10,11,12,13,14 Electron microscopy studies revealed focal myofibrillar disruption, myelin bodies, autophagic vacuoles and mitochondrial abnormalities.5,7,8,10,13,15 Moreover, several reports considered a dense membranous structure surrounding nuclei as being a characteristic ultrastructural feature of MSS7,13,14,16,17 (and MO Livet, personal communication). However, MSS is clinically heterogeneous18 with a marked variation in severity and the occasional presence of the following features: peripheral neuropathy,19,20,21,22,23,24 seizures,10,25 microcephaly, optic atrophy,26 hearing loss,27,28 acute rhabdomyolysis23 and various patterns on magnetic resonance imaging (MRI) such as cerebral atrophy, diffuse reduction of cerebral white matter,25,29 agenesis of the corpus callosum,30 abnormal pituitary gland,25 cyst of the posterior fossa and brainstem atrophy. Moreover, cataract, initially described as congenital, was also found with early childhood onset and rapid progression.9,12,31,32 Different physiopathological hypotheses for MSS were proposed, including lysosomal storage disorder21,33 or defect of chylomicron metabolism,24 but the primary molecular defect remains to be identified.
One major differential diagnosis of MSS is the syndrome defined by congenital cataracts, facial dysmorphism and peripheral neuropathy (CCFDN),34,35,36 which is localised to 18qter37 while no genetic localisation has yet been reported for typical MSS. One subtype of MSS with acute rhabdomyolysis without underlying chronic myopathy23 was shown to be linked to the CCFDN locus,38 suggesting genetic homogeneity between these syndromes. However, we recently showed that MSS and CCFDN are two clinically and genetically distinct entities.16 Using homozygosity mapping strategy, we identified an MSS locus on 5q31 in two large consanguineous families presenting classical features of MS syndrome. On the other hand, linkage to 5q31 was excluded in two families initially diagnosed as MS syndrome, but with the atypical presence of peripheral neuropathy and optic atrophy, and absence of myopathic changes.
Subjects and methods
Subjects
We studied four families with patients presenting characteristic clinical features of MSS and two families with patients presenting an atypical MSS without myopathic changes and including rarely described features such as peripheral neuropathy, optic atrophy or leucoencephalopathy. Clinical features of each patient are summarised in Table 1.
The two patients from family 1, of Turkish origin, are described in detail elsewhere.16,17 Briefly, the affected children were referred to the neuropaediatric clinic due to failure to thrive, reduced head circumference, psychomotor delay, hypotonia and a pronounced ataxic gait and limb ataxia. The disease progression was characterised by the occurrence of bilateral cataracts operated at 4.5 and 6.5 years of age, respectively, and of skeletal deformities secondary to severe hypotonia and muscle weakness. Biological investigations revealed slightly increased serum creatine kinase levels and hypergonadotropic hypogonadism. MRI of the brain revealed isolated marked cerebellar atrophy predominantly affecting the vermis. Muscle biopsy of the two siblings were characterised in both cases by myopathic changes, including variation in muscle fibre size, rimmed vacuoles as well as rare necrotic and regenerating fibres. Electron microscopy disclosed several dense membranous structures surrounding myonuclei, previously reported as specific ultrastructural features of MSS by Sewry et al.7
Families 2–4 are of Norwegian origin. Family 2, originating from the Northern most county of Norway (Finnmark), is a large family with four affected siblings born from second-degree consanguineous parents and two affected cousins. DNA samples of all six patients and a healthy sibling were available for study. This family has been extensively reported in previous publications with regard to clinical picture, biochemical features and myopathic abnormalities.8,15,39,40,41,42,43,44 The patients were followed up for more than 40 years and are 56, 54, 53, 52, 74 and 72 years of age, respectively, at the time of our report. Briefly, all six affected presented characteristic features of MSS including bilateral cataracts, mild mental retardation, hypotonia and cerebellar ataxia due to cerebellar hypoplasia. The short stature and the hypergonadotrophic hypogonadism were reported in four and two of them, respectively. Myopathic changes including subsarcolemmal accumulation of abnormal mitochondria of various shapes and sizes were described in all of them except one.8,15,43,44
The parents of families 3 and 4 are not consanguineous and are related neither to each other, nor to family 2. The three Norwegian families originate from separate Northern Norway counties; however, both parents of family 4 originate from the same small island west of the Norwegian coast.
In family 3, DNA samples of two affected siblings and their parents were available for this study. The patients, previously described by Torbergsen et al,15 are 33 and 31 years old at the time of our report. Clinical features were characteristic of classical MSS and are summarised in Table 1. An additional feature, observed on cerebral MRI of patient 2, consisted in atrophy of pons.
In family 4, DNA samples of one affected individual, her two healthy brothers and her parents, were available. The patient was born after normal pregnancy and delivery. Bilateral cataracts were removed within the first year of life. Spasticity, ataxic gait, hypotonia, mild mental retardation and failure to thrive became evident during infancy. At 8 years of age, cerebral MRI demonstrated cerebral atrophy and wide sulci but no cerebellar atrophy. Serum creatine kinase levels were in normal ranges and no muscle biopsy was available from this patient.
In family 5, DNA samples of the affected patient, her six healthy siblings and their mother were available. Consanguinity between the mother and the father parents is excluded as they are of French and Yugoslav origin, respectively. The patient presented an atypical MSS including congenital cataracts with optic atrophy, mild psychomotor delay (IQ: 76 at 34 years of age), bilateral hearing impairment, hypotonia in infancy, cerebellar ataxia, pyramidal signs and sensitivo-motor demyelinating peripheral neuropathy. Skeletal deformities developed during childhood with dorsal kyphoscoliosis and foot deformities (pes cavus and equino varus). The clinical course was also complicated by partial seizures. Brain MRI revealed cerebellar and diffuse cerebral atrophy. Serum creatine kinase levels were in the normal range and a muscle biopsy did not reveal any myopathic change but only neurogenic muscular atrophy. Electron microscopy did not disclose dense membranous structures characteristic of MSS.
In family 6, of Italian origin, two affected siblings born from nonconsanguineous healthy parents were referred to the neuropaediatric clinic due to psychomotor delay, microcephaly, spasticity, early-onset ataxia and congenital cataracts with macular degeneration. They were diagnosed as presenting an MSS because of the association of cataracts, mental retardation, cerebellar ataxia and skelettal deformities, but they differed clinically from classical MS patients by the presence of microcornea, optic atrophy, insulin-dependent diabetes mellitus and sensory–motor axonal neuropathy. Moreover, brain MRI showed cerebellar and bulbar hypoplasia associated with thin corpus callosum and mild leucoencephalopathy. Serum creatine kinase levels were with normal limits and a muscle biopsy showed only mild neurogenic changes. Serum vitamin E and α-fetoprotein levels were normal. Molecular testing for Friedreich's ataxia and mtDNA mutations were negative.
Genotyping
Blood samples were obtained with informed consent. Genomic DNA was extracted from the peripheral blood leucocytes by a standard phenol/chloroform method.
Whole-genome screens was performed for family 1 using a microsatellite marker set developed and commercialised by PE Biosystems Div. (ABI Linkage Mapping Set version 2, Medium density set 10, MD-10). This set comprises 400 fluorescent-labelled microsatellite markers selected from the Généthon human linkage map45, with an average spacing of 10 cM and an average heterozygosity of 75%.
PCR-multiplex protocols were developed allowing the coamplification of up to six of these markers in a single reaction. For each microsatellite, one primer of the primer set was labelled with one of the three fluorescent dyes (FAMTM, HEXTM, NEDTM) in order to pool PCR products for separation on automatic sequencers. The internal size standard was fluorescently labelled with a fourth dye (ET-ROXTM 400, Amersham Biosciences). All PCR reaction mixes were prepared with a 96-tip head Automation Partnership BasePlate liquid handling robot. PCR were carried out with 20 ng of DNA and the total volume of PCR reaction was 10 μl. PCR were performed with dual 384-well GeneAmp PCR 9700 systems (Applied Biosytems) according to conditions and thermal cycler programmes.
The PCR fragments obtained were pooled and purified on a 96-well MulticreenTM plate by Sephadex G50. A volume of 2 μl of the purified product were transferred to a 96-well plate and mixed with 3 μl of MegaBace loading cocktail (for one reaction: 2.75 μl H2O+0.25 μl ET-ROXTM 400).
The purified dye-labelled fragments were separated according to size on Amersham Biosciences MegaBACE 1000 96-capillary sequencers. The samples were loaded on matrix filled capillaries by electrokinetic injection onto the MegaBace 1000 and ran for 65 min, at 10 kV, using the data collection software (Instrument Control Manager, version 2.1).
Additional CA/TG microsatellite markers from the Généthon human linkage map45 and marker D18S139036,38 amplified by the forward primer 5′-AACGGTTTGGTATTTCCTCA-3′ and the reverse primer 3′-CAGTTCAACAAGGGATTTGG-5′, were analysed on an automated DNA sequencer with a universal fluoresceinated primer, ComF (5′-TAC GCA TCC CAG TTT GAG ACG-3′) as follows.46 Each microsatellite marker was amplified in a three primer PCR reaction in which one of the two specific primers was tailed with the sequence corresponding to the universal fluorescent primer (Spe2+com). A 10:1 molar ratio of primers ComF to Spe2+com was used to ensure that primer Spe2+com is exhausted during the early amplification cycles (Figure 1). The universal primer can be labelled with different fluorochromes, allowing the analysis of several markers of the same size range in a single electrophoretic run.
Method for microsatellite marker genotyping with a universal fluoresceinated primer. Spe1: Specific flanking primer 1. Spe2+Com: Specific flanking primer two tailed with the sequence corresponding to the universal fluorescent primer Com. ComF: universal fluoresceinated primer. In the early amplification cycles, the locus specific primers Spe1 and Spe2+Com yield a specific PCR product containing the tail. A 10:1 molar ratio of primers ComF to Spe2+Com ensures that primer Spe2+Com is exhausted during the early amplification cycles.
PCR reactions were performed in a 25 μl final volume using 50 ng of template DNA, 0.4 μ M of primers Spe1 and ComF and 0.04 μ M of Spe2+com, 1 U of Taq polymerase (Sigma), and 5 μl of buffer (10 mM Tris-HCl pH: 8.3; 50 mM KCl; 200 μ M of each deoxynucleotide triphosphate; 1.5 mM MgCl2). PCR amplification consisted of 35 cycles (94°C for 10 s, 50°C–60°C for 15 s, 72°C for 20 s). PCR products were resolved on an ABI 377 DNA sequencer (PE Applied Biosystems) and analysed using ABI PRISM GeneScan Analysis Software.
Linkage analysis
Part of the linkage power of families 1 and 2 resides in the consanguinity loop(s) and linkage is supported when the patients are homozygous for a rare haplotype.47 This information was included in a two-point LOD score calculation by considering the nonrecombinant haplotype as a single locus.47 Homozygosity by descent found in families with nondocumented consanguinity was computed as second-degree consanguinity, therefore yielding a minimal estimation of the LOD score. The frequency of the homozygous haplotype was calculated as the product of the frequency of the individual alleles estimated from a reference Caucasian population. In order to eliminate biases due to possible linkage disequilibrium, only one marker was taken into account when two were less than 500 kb apart on the human genome sequence working draft. Two-point LOD scores with consanguinity loops were calculated by using the MLINK program of the FASTLINK package.48 We assumed a fully penetrant autosomal recessive mode of inheritance, and a gene frequency of 0.001 that certainly represents an upper limit for this rare condition.
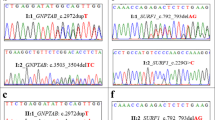
Sequence analysis
The coding sequences of the SARA2 gene were PCR amplified with the following primer pairs: exon 1 F: ATGGGGTGTTCCTTTCTCG and R: GCATGGATGA GACCTGTCCT; exon 2 F: AGATGATCCACCCACCTCAG and R: AGCATTAAAGCATATAGGTAAACTAGC; exon 3 F: GGTTTAGAACTTCAAGCTTAATTGG and R: CTGGGCAA CAGAGAAAGACC; exon 4 F: TGACCTAATGCTTGCTTG GA and R: AGAATCTTACCTTGAACATGT; exon 5 F: ACTTGCCCACAGTCAAGGAA and R: TGCAGAAAAGCTG CACTCTG; exon 6 F: AAGGTGCTGGCTCTATACGTTC and R: AATGGGCTTGTATAGTTGGACA; exon 7 F: GCAGC CACGACTTTATCACA and R: GCTGGGGTGATGTCAGAT TA. PCR products were purified on Montage PCR96 Cleanup Plates (Millipore, Bedford, MA, USA) and used in sequencing reactions with the ABI BigDye terminator kit (Applied Biosystems, Foster City, CA, USA), which were subsequently run on an ABI PRISM 3100 Genetic Analyzer.
Results
A total of 391 markers of the ABI PRISM Linkage Mapping Set were tested on family 1. Given the close consanguinity of the parents and the close spacing of the markers, we selected the regions for which at least one marker was homozygous in both affected individuals and heterozygous in the four healthy siblings. We identified four such regions. New flanking markers were tested for each region and haplotypes were constructed. This allowed us to exclude linkage for two of the four regions, whereas 15 and five consecutive markers were found homozygous at loci 5q31 (Figure 2) and 7p14.2, thereby defining two potential regions of linkage.
Linkage of the disease to the 5q31 region in families 1 (a) and 2 (b). Markers are indicated on the left and are organised from top to bottom in the centromeric to telomeric order. Parental haplotypes linked with the disease are boxed. The region of consanguinity by descent is boxed in grey. The homozygous markers D5S2115, −399 and -479 in the healthy daughter of family 1 are not informative in her mother, and therefore do not allow to position precisely the critical recombination breakpoint. Allele 130 of marker D5S2017 in the second daughter of family 2 is assumed to be a de novo mutation from a 126 allele. The grand parents of patients 5 and 6 are known not to be brother and sister or uncle and niece/aunt and nephew. Therefore, the closest possible consanguinity between these grand parents would be second degree, which was used for a minimal estimation of the LOD score (see Subjects and methods).
The study of a dense set of microsatellite markers from the two regions45 in family 2, allowed us to exclude linkage to the 7p14.2 locus and confirmed linkage to the 5q31 locus, since the six patients were homozygous for at least eight consecutive markers and the healthy sibling was heterozygous for seven of these markers (Figure 2). The recombinant markers D5S1995 (centromeric) and D5S436 (distal) defined a 9.3 cM interval, which is included in the 5q31 region of linkage of family 1. LOD score calculation, including the consanguinity loops,47,49 gave a value of 2.9 and 5.6 for families 1 and 2, respectively, at a recombination fraction θ of 0, indicating linkage between the disease and the 5q31 haplotype.
Segregation of the 5q31 locus in the two small Norwegian families (families 3 and 4) was compatible with linkage to the disease (Figure 3). However, families 3 and 4 had heterozygous linked haplotypes and shared no common haplotype, either with respect to each other or with respect to family 2. Finally, linkage of the disease to 5q31 was excluded in families 5 and 6, of French and Italian origin, respectively (Figure 4). Indeed, the affected individual of family 5 shared identical haplotypes over the entire region with two healthy siblings. In family 6, the two patients were discordant over the entire region and patient 2 shared identical haplotypes with his healthy sister. Since the patients of these two families presented with atypical MSS features including peripheral neuropathy without chronic myopathy, we tested the families with markers D18S1122, D18S70 and D18S1390 of the CCFDN-MSS/myoglobinuria locus. Linkage of the disease to 18qter was also excluded for the two families (data not shown).
While this work was under review, Jones et al50 reported the identification of disease causing mutations in the SARA2 gene of patients with chylomicron retention disease (CRMD), including one family where CRMD cosegregates with MSS in two brothers. Since the SARA2 gene lies in our MSS critical interval, we searched for mutations in the SARA2 gene of the Turkish and Norvegian families (families 1–4). A silent nucleotide change (133C → T, S45S) was found in the affected children of the Turkish family and a 895A → G polymorphism was found in the 3′UTR of the SARA2 gene in the healthy sibling of family 2 and in the patients of family 3.
Discussion
We demonstrate in this study that MSS in the two consanguineous families 1 and 2 is linked to a 9.3 cM region on 5q31 defined by the flanking markers D5S1995 and D5S436. The LOD score in favour of linkage in family 2, firmly establishes the MSS locus to 5q31 for this family. The LOD score in favour of linkage in family 1 is well above the 2.56 threshold corresponding to a posterior probability of 95% for linkage of family 1 to the same locus as family 2.49 On the other hand, the disease in families 5 and 6 is clearly excluded from the 5q31 locus, allowing to the distinction between the two entities. The patients of the 5q31 linked families have typical MSS defined by congenital cerebellar ataxia with cerebellar atrophy and hypotonia, early-onset cataracts (not necessarily congenital), psychomotor and growth delay, hypergonadotrophic hypogonadism and myopathic changes on muscle biopsy. Several such patients have been previously reported in the literature.5,6,7,9,10,11,12,13,14 We propose that, for the sake of genetic counselling and in the absence of identified defective gene and mutations, the syndrome of Marinesco–Sjögren is restricted to these typical patients. With such criteria, family 3 appears to have MSS, in agreement with the sharing of both parental haplotypes of the two patients. The patients with cerebellar ataxia, cataracts and psychomotor delay but without the myopathic changes are not linked to 5q31 and have (a) distinct disease(s) that associate(s) additional features, including peripheral neuropathy, optic atrophy and various combinations of deafness, seizures, cerebral atrophy, microcephaly, leucoencephalopathy, microcornea and diabetes mellitus. These patients have a disease more akin to the CCFDN syndrome,16,34,35,36,37 yet distinct, since it does not segregate with the CCFDN locus on 18qter. Moreover, the absence of mutation in the SARA2 gene of the 5q31 linked families indicates either that the CMRD-MSS syndrome (OMIM 607692) is a nonallelic genetic entity distinct from typical MSS, or that, given the close proximity of the CMRD and MSS loci, the two diseases cosegregrate by chance in the unique family reported by Aguglia et al.24
We have shown here that there is at least three different genes that result in cataract, cerebellar ataxia and mental and growth retardation, when defective, suggesting that a complex pathway involving several participating proteins might be defective in these diseases. It appears that the myopathic changes seen on muscle biopsy are an important feature of the pathology of MSS. The exact nature of these changes remains controversial. They include characteristic perinuclear membrane inclusions,7,13,14,16 subsarcolemnal rimmed vacuoles,5,6,7,10,11,12,13,14,16 abnormal mitochondria5,7,8,10,13,15 and rarely ragged red fibres.8,15 Albeit an OXPHOS deficiency has been excluded in several MSS patients, the possibility that a mitochondrial defect underlies the pathogenesis of MSS is an attractive hypothesis, since combination of neurodegeneration and myopathy is often seen in mitochondrial diseases.51 The identification of the MSS locus represents a first step towards the identification of the defective gene and therefore the testing of this hypothesis.
References
Marinesco G, Draganesco S, Vasiliu D : Nouvelle maladie familiale caractérisée par une cataracte congénitale et un arrêt du développement somato-neuro-psychique. L’encéphale 1931; 26: 97–109.
Sjögren T : Hereditary congenital spinocerebellar ataxia accompanied by congenital cataract and oligophrenia. Confinia Neurol 1950; 10: 293–308.
Brogdon BG, Snow RD, Williams JP : Skeletal findings in Marinesco–Sjogren syndrome. Skeletal Radiol 1996; 25: 461–465.
Reinker K, Hsia YE, Rimoin DL et al: Orthopaedic manifestations of Marinesco–Sjogren syndrome. J Pediatr Orthop 2002; 22: 399–403.
Superneau DW, Wertelecki W, Zellweger H, Bastian F : Myopathy in Marinesco–Sjogren syndrome. Eur Neurol 1987; 26: 8–16.
Herva R, von Wendt L, von Wendt G, Saukkonen AL, Leisti J, Dubowitz V : A syndrome with juvenile cataract, cerebellar atrophy, mental retardation and myopathy. Neuropediatrics 1987; 18: 164–169.
Sewry CA, Voit T, Dubowitz V : Myopathy with unique ultrastructural feature in Marinesco–Sjogren syndrome. Ann Neurol 1988; 24: 576–580.
Borud O, Aasly J, Lindal S : Mitochondrial myopathy in six patients with Marinesco–Sjogren syndrome. Prog Clin Biol Res 1989; 306: 135–139.
Komiyama A, Nonaka I, Hirayama K : Muscle pathology in Marinesco–Sjogren syndrome. J Neurol Sci 1989; 89: 103–113.
Goto Y, Komiyama A, Tanabe Y, Katafuchi Y, Ohtaki E, Nonaka I : Myopathy in Marinesco–Sjogren syndrome: an ultrastructural study. Acta Neuropathol 1990; 80: 123–128.
Kodama S, Komatsu M, Miyoshi M, Nakao H, Sakurai T : Marinesco–Sjogren syndrome with reduced cytochrome c oxidase in muscle. Kobe J Med Sci 1992; 38: 245–254.
Ishikawa T, Kitoh H, Awaya A, Nonaka I : Rapid cataract formation in Marinesco–Sjogren syndrome. Pediatr Neurol 1993; 9: 407–408.
Sasaki K, Suga K, Tsugawa S et al: Muscle pathology in Marinesco–Sjogren syndrome: a unique ultrastructural feature. Brain Dev 1996; 18: 64–67.
Suzuki Y, Murakami N, Goto Y et al: Apoptotic nuclear degeneration in Marinesco–Sjogren syndrome. Acta Neuropathol (Berl) 1997; 94: 410–415.
Torbergsen T, Aasly J, Borud O, Lindal S, Mellgren SI : Mitochondrial myopathy in Marinesco–Sjogren syndrome. J Ment Defic Res 1991; 35: 154–159.
Lagier-Tourenne C, Chaigne D, Gong J et al: Linkage to 18qter differentiates two clinically overlapping syndromes: Congenital Cataracts Facial Dysmorphism Neuropathy syndrome and Marinesco-Sjögren syndrome. J Med Genet 2002; 39: 838–843.
Chaigne D, Mohr M, Bintner M : Myopathie et syndrome de Marinesco et Sjögren. A propos d’une observation familiale. Rev Neurol (Paris) 1993; 149: A238.
Williams TE, Buchhalter JR, Sussman MD : Cerebellar dysplasia and unilateral cataract in Marinesco–Sjogren syndrome. Pediatr Neurol 1996; 14: 158–161.
Hakamada S, Sobue G, Watanabe K, Kumagai T, Hara K, Miyazaki S : Peripheral neuropathy in Marinesco–Sjogren syndrome. Brain Dev 1981; 3: 403–406.
Alexianu M, Christodorescu D, Vasilescu C et al: Sensorimotor neuropathy in a patient with Marinesco–Sjogren syndrome. Eur Neurol 1983; 22: 222–226.
Zimmer C, Gosztonyi G, Cervos-Navarro J, von Moers A, Schroder JM : Neuropathy with lysosomal changes in Marinesco–Sjogren syndrome: fine structural findings in skeletal muscle and conjunctiva. Neuropediatrics 1992; 23: 329–335.
Farah S, Sabry MA, Khuraibet AJ et al: Marinesco–Sjogren syndrome in a Bedouin family. Acta Neurol Scand 1997; 96: 387–391.
Muller-Felber W, Zafiriou D, Scheck R et al: Marinesco–Sjogren syndrome with rhabdomyolysis. A new subtype of the disease. Neuropediatrics 1998; 29: 97–101.
Aguglia U, Annesi G, Pasquinelli G et al: Vitamin E deficiency due to chylomicron retention disease in Marinesco–Sjogren syndrome. Ann Neurol 2000; 47: 260–264.
McLaughlin JF, Pagon RA, Weinberger E, Haas JE : Marinesco–Sjogren syndrome: clinical and magnetic resonance imaging features in three children. Dev Med Child Neurol 1996; 38: 636–644.
Dotti MT, Bardelli AM, De Stefano N et al: Optic atrophy in Marinesco–Sjogren syndrome: an additional ocular feature. Report of three cases in two families. Ophthalm Paediatr Genet 1993; 14: 5–7.
Begeer JH, Scholte FA, van Essen AJ : Two sisters with mental retardation, cataract, ataxia, progressive hearing loss, and polyneuropathy. J Med Genet 1991; 28: 884–885.
Newton VE : Sensorineural hearing loss and the Marinesco–Sjogren syndrome. J Laryngol Otol 1991; 105: 210–212.
Bromberg MB, Junck L, Gebarski SS, McLean MJ, Gilman S : The Marinesco–Sjogren syndrome examined by computed tomography, magnetic resonance, and 18F-2-fluoro-2-deoxy-D-glucose and positron emission tomography. Arch Neurol 1990; 47: 1239–1242.
Georgy BA, Snow RD, Brogdon BG, Wertelecki W : Neuroradiologic findings in Marinesco–Sjogren syndrome. Am J Neuroradiol 1998; 19: 281–283.
Alter M, Kennedy W : The Marinesco–Sjogren syndrome. Hereditary cerebello-lental degeneration with mental retardation. Minn Med 1968; 51: 901–906.
Tachi N, Nagata N, Wakai S, Chiba S : Congenital muscular dystrophy in Marinesco–Sjogren syndrome. Pediatr Neurol 1991; 7: 296–298.
Walker PD, Blitzer MG, Shapira E : Marinesco–Sjogren syndrome: evidence for a lysosomal storage disorder. Neurology 1985; 35: 415–419.
Tournev I, Kalaydjieva L, Youl B et al: Congenital cataracts facial dysmorphism neuropathy syndrome, a novel complex genetic disease in Balkan Gypsies: clinical and electrophysiological observations. Ann Neurol 1999; 45: 742–750.
Tournev I, King RH, Workman J et al: Peripheral nerve abnormalities in the congenital cataracts facial dysmorphism neuropathy (CCFDN) syndrome. Acta Neuropathol (Berl) 1999; 98: 165–170.
Tournev I, Thomas PK, Gooding R et al: Congenital cataracts facial dysmorphism neuropathy syndrome – clinical, neuropathological and genetic investigation. Acta Myolog 2001; XX: 210–219.
Angelicheva D, Turnev I, Dye D, Chandler D, Thomas PK, Kalaydjieva L : Congenital cataracts facial dysmorphism neuropathy (CCFDN) syndrome: a novel developmental disorder in Gypsies maps to 18qter. Eur J Hum Genet 1999; 7: 560–566.
Merlini L, Gooding R, Lochmuller H et al: Genetic identity of Marinesco–Sjogren/myoglobinuria and CCFDN syndromes. Neurology 2002; 58: 231–236.
Bassöe HH : Familial congenital muscular dystrophy with gonadal dysgenesis. J Clin Endocrinol 1956; 16: 1614–1621.
Andersen B : Spinocerebellar ataxia, congenital cataract, somatic and mental retardation. Dev Med Child Neurol 1965; 7: 249–257.
Skre H, Bassöe HH, Berg K, Frövig AG : Cerebellar ataxia and hypergonadotropic hypogonadism in two kindreds. Chance concurrence, pleiotropism or linkage? Clin Genet 1976; 9: 234–244.
Skre H, Berg K : Linkage studies on Marinesco–Sjogren syndrome and hypergonadotropic hypogonadism. Clin Genet 1977; 11: 57–66.
Torbergsen T, Stalberg E, Aasly J, Lindal S : Myopathy in Marinesco–Sjogren syndrome: an electrophysiological study. Acta Neurol Scand 1991; 84: 132–138.
Lindal S, Lund I, Torbergsen T et al: Mitochondrial diseases and myopathies: a series of muscle biopsy specimens with ultrastructural changes in the mitochondria. Ultrastruct Pathol 1992; 16: 263–275.
Dib C, Faure S, Fizames C et al: A comprehensive genetic map of the human genome based on 5264 microsatellites. Nature 1996; 380: 152–154.
Warner JP, Barron LH, Goudie D et al: A general method for the detection of large CAG repeat expansions by fluorescent PCR. J Med Genet 1996; 33: 1022–1026.
Ben Hamida C, Doerflinger N, Belal S et al: Localization of Friedreich ataxia phenotype with selective vitamin E deficiency to chromosome 8q by homozygosity mapping. Nat Genet 1993; 5: 195–200.
Cottingham RW, Idury RM, Schaffer AA : Faster sequential genetic linkage computations. Am J Hum Genet 1993; 53: 252–263.
Lathrop GM, Lalouel JM, Julier C, Ott J : Multilocus linkage analysis in humans: detection of linkage and estimation of recombination. Am J Hum Genet 1985; 37: 482–498.
Jones B, Jones EL, Bonney SA et al: Mutations in a Sar1 GTPase of COPII vesicles are associated with lipid absorption disorders. Nat Genet 2003; 34: 29–31.
Schon EA, Manfredi G : Neuronal degeneration and mitochondrial dysfunction. J Clin Invest 2003; 111: 303–312.
Acknowledgements
We thank all patients and families for their collaboration. We are indebt to Professor J-L Mandel for continued encouragement and helpful discussions, and Maria-Céu Moreira for sharing her time and experience. We wish to thank Dr M-E Valente and Dr C Jonsrud for referring DNA samples of the Italian and Norwegian families, respectively. We thank I Colas, E Troesch, F Ruffenach and S Vicaire for excellent technical help. Genetic studies were supported by funds from the Institut National de la Santé et de la Recherche Médicale, the Centre National de la Recherche Scientifique, the GIS Maladies Rares and the Hôpitaux Universitaires de Strasbourg (PHRC regional). CL-T was supported by the Association Française contre les Myopathies and by the Fondation pour la Recherche Médicale.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lagier-Tourenne, C., Tranebjærg, L., Chaigne, D. et al. Homozygosity mapping of Marinesco–Sjögren syndrome to 5q31. Eur J Hum Genet 11, 770–778 (2003). https://doi.org/10.1038/sj.ejhg.5201068
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201068