Summary
Women live longer than men and develop cardiovascular disease (CVD) at an older age. The metabolic syndrome represents a major risk factor for the development of CVD, and gender1 differences in this syndrome may contribute to gender differences in CVD.
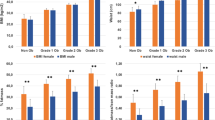
In recent years, the metabolic syndrome has been more prevalent in men than in women. Prevalence is increasing and this increase has been steeper in women, particularly in young women, during the last decade. The contributions of the different components of the metabolic syndrome differ between genders and in different countries.
In a recent survey in Germany, 40% of the adult population had been diagnosed with disturbed glucose tolerance or type 2 diabetes. Undiagnosed diabetes was more frequent in men than in women, and risk factors for undiagnosed diabetes differed between the sexes. Worldwide, in individuals with impaired glucose tolerance, impaired fasting glucose was observed more frequently in men, whereas impaired glucose tolerance occurred relatively more often in women. Lipid accumulation patterns differ between women and men. Premenopausal women more frequently develop peripheral obesity with subcutaneous fat accumulation, whereas men and postmenopausal women are more prone to central or android obesity. In particular, android obesity is associated with increased cardiovascular mortality and the development of type 2 diabetes. Visceral adipocytes differ from peripheral adipocytes in their lipolytic activity and their response to insulin, adrenergic and angiotensin stimulation and sex hormones. Visceral fat is a major source of circulating free fatty acids and cytokines, which are directly delivered via the portal vein to the liver inducing insulin resistance and an atherogenic lipid profile. Inflammation increases cardiovascular risk particularly in women. A relatively greater increase in cardiovascular risk by the appearance of diabetes in women has been reported in many studies.
Thus, the presently available data suggest that the pathophysiology of the metabolic syndrome and its contribution to the relative risk of cardiovascular events and heart failure show gender differences, which might be of potential relevance for prevention, diagnostics, and therapy of the syndrome.
Similar content being viewed by others
References
Crepaldi G, Tiengo A (1976) Hyperlipoproteinemia and diabetes. Minerva Med 67(4):290–300
Eckel RH, Grundy SM, Zimmet PZ (2005) The metabolic syndrome. Lancet 365(9468):1415–1428
Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C (2004) Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 109(3):433– 438
Lorenzo C, Okoloise M, Williams K, Stern MP, Haffner SM (2003) The metabolic syndrome as predictor of type 2 diabetes: the San Antonio heart study. Diabetes Care 26(11):3153–3159
Alexander CM, Landsman PB, Teutsch SM, Haffner SM (2003) NCEP–defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes 52(5):1210–1214
Ford ES, Giles WH, Dietz WH (2002) Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. Jama 287(3):356–359
Balkau B, Charles MA, Drivsholm T, Borch–Johnsen K, Wareham N, Yudkin JS et al (2002) Frequency of the WHO metabolic syndrome in European cohorts, and an alternative definition of an insulin resistance syndrome. Diabetes Metab 28(5):364–376
Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP (2001) The continuing epidemics of obesity and diabetes in the United States. Jama 286(10):1195–1200
Koenig W (1998) Epidemiology of coronary heart disease. Z Kardiol 87(Suppl 2):3–7
Ford ES, Giles WH, Mokdad AH (2004) Increasing prevalence of the metabolic syndrome among u. s. Adults. Diabetes Care 27(10):2444– 2449
Steinbaum SR (2004) The metabolic syndrome: an emerging health epidemic in women. Prog Cardiovasc Dis 46(4):321–336
Williams JW, Zimmet PZ, Shaw JE, de Courten MP, Cameron AJ, Chitson P et al (2003) Gender differences in the prevalence of impaired fasting glycaemia and impaired glucose tolerance in Mauritius. Does sex matter? Diabet Med 20(11):915–920
Dallongeville J, Cottel D, Arveiler D, Tauber JP, Bingham A, Wagner A et al (2004) The association of metabolic disorders with the metabolic syndrome is different in men and women. Ann Nutr Metab 48(1):43–50
Wajchenberg BL (2000) Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev 21(6):697–738
Zhu S, St–Onge MP, Heshka S, Heymsfield SB (2004) Lifestyle behaviors associated with lower risk of having the metabolic syndrome. Metabolism 53(11):1503–1511
Rathmann W, Haastert B, Icks A, Lowel H, Meisinger C, Holle R et al (2003) High prevalence of undiagnosed diabetes mellitus in Southern Germany: target populations for efficient screening. The KORA survey 2000. Diabetologia 46(2):182–189
Hanefeld M, Koehler C, Fuecker K, Henkel E, Schaper F, Temelkova– Kurktschiev T (2003) Insulin secretion and insulin sensitivity pattern is different in isolated impaired glucose tolerance and impaired fasting glucose: the risk factor in Impaired Glucose Tolerance for Atherosclerosis and Diabetes study. Diabetes Care 26(3):868–874
Enbergs A, Liese A, Heimbach M, Kerber S, Scheld HH, Breithardt G et al (1997) Evaluation of secondary prevention of coronary heart disease. Results of the EUROSPIRE study in the Munster region. Z Kardiol 86(4):284–291
Pomerleau J, McKeigue PM, Chaturvedi N (1999) Relationships of fasting and postload glucose levels to sex and alcohol consumption. Are American Diabetes Association criteria biased against detection of diabetes in women? Diabetes Care 22(3):430– 433
Falkner B, Hulman S, Kushner H (1994) Gender differences in insulinstimulated glucose utilization among African–Americans. Am J Hypertens 7(11):948–952
Travers SH, Jeffers BW, Eckel RH (2002) Insulin resistance during puberty and future fat accumulation. J Clin Endocrinol Metab 87(8):3814– 3818
Regitz–Zagrosek V, Lehmkuhl E, Hocher B, Goesmann D, Lehmkuhl HB, Hausmann H et al (2004) Gender as a risk factor in young, not in old, women undergoing coronary artery bypass grafting. J Am Coll Cardiol 44(12):2413–2414
Goldstein BJ (2002) Insulin resistance as the core defect in type 2 diabetes mellitus. Am J Cardiol 90(5A):3G– 10G
Muller–Wieland D, Kotzka J, Knebel B, Krone W (1998) Metabolic syndrome and hypertension: pathophysiology and molecular basis of insulin resistance. Basic Res Cardiol 93(Suppl 2):131–134
Murphy MJ, Metcalf BS, Voss LD, Jeffery AN, Kirkby J, Mallam KM et al (2004) Girls at five are intrinsically more insulin resistant than boys: The Programming Hypotheses Revisited – The EarlyBird Study (EarlyBird 6). Pediatrics 113(1 Pt 1):82–86
Moran A, Jacobs DR Jr, Steinberger J, Hong CP, Prineas R, Luepker R et al (1999) Insulin resistance during puberty: results from clamp studies in 357 children. Diabetes 48(10):2039– 2044
Ehm MG, Karnoub MC, Sakul H, Gottschalk K, Holt DC, Weber JL et al (2000) Genomewide search for type 2 diabetes susceptibility genes in four American populations. Am J Hum Genet 66(6):1871–1881
Barrett–Connor E, Ferrara A (1998) Isolated postchallenge hyperglycemia and the risk of fatal cardiovascular disease in older women and men. The Rancho Bernardo Study. Diabetes Care 21(8):1236–1239
Valve R, Sivenius K, Miettinen R, Pihlajamaki J, Rissanen A, Deeb SS et al (1999) Two polymorphisms in the peroxisome proliferator–activated receptor– gamma gene are associated with severe overweight among obese women. J Clin Endocrinol Metab 84(10):3708–3712
Williams CM (2004) Lipid metabolism in women. Proc Nutr Soc 63(1):153–160
Lonnqvist F, Thorne A, Large V, Arner P (1997) Sex differences in visceral fat lipolysis and metabolic complications of obesity. Arterioscler Thromb Vasc Biol 17(7):1472–1480
Pedersen SB, Kristensen K, Hermann PA, Katzenellenbogen JA, Richelsen B (2004) Estrogen controls lipolysis by up–regulating alpha2A–adrenergic receptors directly in human adipose tissue through the estrogen receptor alpha. Implications for the female fat distribution. J Clin Endocrinol Metab 89(4):1869–1878
Bjorntorp P (2000) Metabolic difference between visceral fat and subcutaneous abdominal fat. Diabetes Metab 26(Suppl 3):10–12
Krotkiewski M, Bjorntorp P, Sjostrom L, Smith U (1983) Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J Clin Invest 72(3):1150– 1162
Mayes JS, Watson GH (2004) Direct effects of sex steroid hormones on adipose tissues and obesity. Obes Rev 5(4):197–216
Huang KC, Lin RC, Kormas N, Lee LT, Chen CY, Gill TP et al (2004) Plasma leptin is associated with insulin resistance independent of age, body mass index, fat mass, lipids, and pubertal development in nondiabetic adolescents. Int J Obes Relat Metab Disord 28(4):470–475
Steinberger J, Steffen L, Jacobs DR Jr, Moran A, Hong CP, Sinaiko AR (2003) Relation of leptin to insulin resistance syndrome in children. Obes Res 11(9):1124–1130
Van Harmelen V, Reynisdottir S, Eriksson P, Thorne A, Hoffstedt J, Lonnqvist F et al (1998) Leptin secretion from subcutaneous and visceral adipose tissue in women. Diabetes 47(6):913–917
Montague CT, Prins JB, Sanders L, Digby JE, O‘Rahilly S (1997) Depotand sex–specific differences in human leptin mRNA expression: implications for the control of regional fat distribution. Diabetes 46(3):342–347
Ryo M, Nakamura T, Kihara S, Kumada M, Shibazaki S, Takahashi M et al (2004) Adiponectin as a biomarker of the metabolic syndrome. Circ J 68(11):975–981
Costacou T, Zgibor JC, Evans RW, Otvos J, Lopes–Virella MF, Tracy RP et al (2004) The prospective association between adiponectin and coronary artery disease among individuals with type 1 diabetes. The Pittsburgh Epidemiology of Diabetes Complications Study. Diabetologia 23:23
Kougias P, Chai H, Lin PH, Lumsden AB, Yao Q, Chen C (2005) Adipocytederived cytokine resistin causes endothelial dysfunction of porcine coronary arteries. J Vasc Surg 41(4):691– 698
Banerjee RR, Lazar MA (2003) Resistin: molecular history and prognosis. J Mol Med 81(4):218–226
Yannakoulia M, Yiannakouris N, Bluher S, Matalas AL, Klimis–Zacas D, Mantzoros CS (2003) Body fat mass and macronutrient intake in relation to circulating soluble leptin receptor, free leptin index, adiponectin, and resistin concentrations in healthy humans. J Clin Endocrinol Metab 88(4):1730–1736
Lewandowski KC, Szosland K, O‘Callaghan C, Tan BK, Randeva HS, Lewinski A (2005) Adiponectin and resistin serum levels in women with polycystic ovary syndrome during oral glucose tolerance test: a significant reciprocal correlation between adiponectin and resistin independent of insulin resistance indices. Mol Genet Metab 85(1):61–69
Bertolini S, Pisciotta L, Di Scala L, Langheim S, Bellocchio A, Masturzo P et al (2004) Genetic polymorphisms affecting the phenotypic expression of familial hypercholesterolemia. Atherosclerosis 174(1):57–65
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML et al (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women‘s Health Initiative randomized controlled trial. Jama 288(3):321–333
Clarke SC, Kelleher J, Lloyd–Jones H, Slack M, Schofiel PM (2002) A study of hormone replacement therapy in postmenopausal women with ischemic heart disease: the Papworth HRT atherosclerosis study. Bjog 109(9):1056–1062
Cheurfa N, Reis AF, Dubois–Laforgue D, Bellanne–Chantelot C, Timsit J, Velho G (2004) The Gly482Ser polymorphism in the peroxisome proliferator– activated receptor–gamma coactivator– 1 gene is associated with hypertension in type 2 diabetic men. Diabetologia 47(11):1980–1983
Oberkofler H, Holzl B, Esterbauer H, Xie M, Iglseder B, Krempler F et al (2003) Peroxisome proliferator–activated receptor–gamma coactivator–1 gene locus: associations with hypertension in middle–aged men. Hypertension 41(2):368–372
Kuznetsova T, Staessen JA, Thijs L, Kunath C, Olszanecka A, Ryabikov A et al (2004) Left ventricular mass in relation to genetic variation in angiotensin II receptors, renin system genes, and sodium excretion. Circulation 110(17):2644–2650
Gasse C, Hense HW, Stieber J, Doring A, Liese AD, Keil U (2001) Assessing hypertension management in the community: trends of prevalence, detection, treatment, and control of hypertension in the MONICA Project, Augsburg 1984–1995. J Hum Hypertens 15(1):27–36
Rahmouni K, Correia ML, HaynesWG, Mark AL (2005) Obesity–associated hypertension: new insights into mechanisms. Hypertension 45(1):9–14
Sironi AM, Gastaldelli A, Mari A, Ciociaro D, Postano V, Buzzigoli E et al (2004) Visceral fat in hypertension: influence on insulin resistance and beta–cell function. Hypertension 44 (2):127–133
Faria AN, Ribeiro Filho FF, Gouveia Ferreira SR, Zanella MT (2002) Impact of visceral fat on blood pressure and insulin sensitivity in hypertensive obese women. Obes Res 10(12):1203–1206
Pechere–Bertschi A, Burnier M (2004) Female sex hormones, salt, and blood pressure regulation. Am J Hypertens 17(10):994–1001
Nickenig G (2004) Should angiotensin II receptor blockers and statins be combined? Circulation 110(8):1013– 1020
Ridker PM, Morrow DA (2003) C–reactive protein, inflammation, and coronary risk. Cardiol Clin 21(3):315–325
Ross R (1999) Atherosclerosis – an inflammatory disease. N Engl J Med 340(2):115–126
Han TS, Sattar N, Williams K, Gonzalez– Villalpando C, Lean ME, Haffner SM (2002) Prospective study of C–reactive protein in relation to the development of diabetes and metabolic syndrome in the Mexico City Diabetes Study. Diabetes Care 25(11):2016–2021
Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM (2001) C–reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. Jama 286(3):327–334
Rutter MK, Meigs JB, Sullivan LM, D’Agostino RB Sr, Wilson PW (2004) C–reactive protein, the metabolic syndrome, and prediction of cardiovascular events in the Framingham Offspring Study. Circulation 110(4):380– 385
Nakanishi N, Shiraishi T, Wada M (2005) C–reactive protein concentration is more strongly related to metabolic syndrome in women than in men: the Minoh Study. Circ J 69(4):386–391
Azziz R (2002) Polycystic ovary syndrome, insulin resistance, and molecular defects of insulin signaling. J Clin Endocrinol Metab 87(9):4085– 4087
Moran L, Norman RJ (2004) Understanding and managing disturbances in insulin metabolism and body weight in women with polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol 18(5):719–736
Gambineri A, Pelusi C, Vicennati V, Pagotto U, Pasquali R (2002) Obesity and the polycystic ovary syndrome. Int J Obes Relat Metab Disord 26(7):883–896
Solomon CG, Hu FB, Dunaif A, Rich– Edwards JE, Stampfer MJ, Willett WC et al (2002) Menstrual cycle irregularity and risk for future cardiovascular disease. J Clin Endocrinol Metab 87(5):2013–2017
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M et al (2001) Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24(4):683– 689
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J et al (2002) The metabolic syndrome and total and cardiovascular disease mortality in middle–aged men. JAMA 288(21):2709–2716
Wilson PW, Kannel WB, Silbershatz H, D’Agostino RB (1999) Clustering of metabolic factors and coronary heart disease. Arch Intern Med 159(10):1104–1109
Sattar N, Gaw A, Scherbakova O, Ford I, O‘Reilly DS, Haffner SM et al (2003) Metabolic syndrome with and without C–reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation 108(4):414–419
Onat A, Ceyhan K, Basar O, Erer B, Toprak S, Sansoy V (2002) Metabolic syndrome: major impact on coronary risk in a population with low cholesterol levels – a prospective and crosssectional evaluation. Atherosclerosis 165(2):285–292
Kip KE, Marroquin OC, Kelley DE, Johnson BD, Kelsey SF, Shaw LJ et al (2004) Clinical importance of obesity versus the metabolic syndrome in cardiovascular risk in women: a report from the Women‘s Ischemia Syndrome Evaluation (WISE) study. Circulation 109(6):706–713
Marroquin OC, Kip KE, Kelley DE, Johnson BD, Shaw LJ, Bairey Merz CN et al (2004) Metabolic syndrome modifies the cardiovascular risk associated with angiographic coronary artery disease in women: a report from the Women‘s Ischemia Syndrome Evaluation. Circulation 109(6):714– 721
Lundberg V, Stegmayr B, Asplund K, Eliasson M, Huhtasaari F (1997) Diabetes as a risk factor for myocardial infarction: population and gender perspectives. J Intern Med 241(6):485–492
Pan WH, Cedres LB, Liu K, Dyer A, Schoenberger JA, Shekelle RB et al (1986) Relationship of clinical diabetes and asymptomatic hyperglycemia to risk of coronary heart disease mortality in men and women. Am J Epidemiol 123(3):504–516
Thompson SG, Kienast J, Pyke SD, Haverkate F, van de Loo JC (1995) Hemostatic factors and the risk of myocardial infarction or sudden death in patients with angina pectoris. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. N Engl J Med 332(10):635–641
Steinberg HO, Paradisi G, Cronin J, Crowde K, Hempfling A, Hook G et al (2000) Type II diabetes abrogates sex differences in endothelial function in premenopausal women. Circulation 101(17):2040–2046
Barrett–Connor EL, Cohn BA, Wingard DL, Edelstein SL (1991) Why is diabetes mellitus a stronger risk factor for fatal ischemic heart disease in women than in men? The Rancho Bernardo Study. Jama 265(5):627–631
Scheidt–Nave C, Barrett–Connor E, Wingard DL, Cohn BA, Edelstein SL (1991) Sex differences in fasting glycemia as a risk factor for ischemic heart disease death. Am J Epidemiol 133(6):565–576
Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG et al (2002) Obesity and the risk of heart failure. N Engl J Med 347(5):305–313
Flegal KM, Carroll MD, Ogden CL, Johnson CL (2002) Prevalence and trends in obesity among US adults, 1999–2000. JAMA 288(14):1723–1727
Peterson LR, Herrero P, Schechtman KB, Racette SB, Waggoner AD, Kisrieva– Ware Z et al (2004) Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation 109(18):2191–2196
Gibbons RJ, Balady GJ, Bricker JT, Chaitman BR, Fletcher GF, Froelicher VF et al (2002) ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation 106(14):1883–1892
Balkau B, Charles MA (1999) Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR). Diabet Med 16(5):442– 443
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15(7):539–553
NCEP (2001) Executive Summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Jama 285(19):2486–2497
Einhorn D, Reaven GM, Cobin RH, Ford E, Ganda OP, Handelsman Y et al (2003) American College of Endocrinology position statement on the insulin resistance syndrome. Endocr Pract 9(3):237–252
Author information
Authors and Affiliations
Corresponding author
Additional information
1 "Gender" is used to include biological sex as well as gender in its strict sense
Supported by the DFG (grants to V. Regitz–Zagrosek) and the BMBF (Competence Network Heart Failure)
An erratum to this article can be found at http://dx.doi.org/10.1007/s00392-006-0377-8
Rights and permissions
About this article
Cite this article
Regitz-Zagrosek, V., Lehmkuhl, E. & Weickert, M.O. Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin Res Cardiol 95, 136–147 (2006). https://doi.org/10.1007/s00392-006-0351-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-006-0351-5