Abstract
Introduction
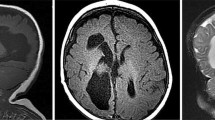
The sophistication of prenatal brain imaging (US, MRI) has awakened interest in fetal neuropathology and changed the concept of brain malformations, defined until recently through descriptive terms and considered as senseless accidents of development. Usually, most CNS malformations are documented from a clinical and radiological point of view. However, only a detailed neuropathological study permits their exact phenotype to be established, which is instrumental for a precise diagnosis and cause analysis.
Discussion
After pregnancy termination for fetal malformations (or prenatal death) full autopsy and frozen tissue storage for DNA analysis are mandatory. The delay between death and autopsy should be limited because of the rapid autolysis of brain tissue. Detailed neuropathological and cause analysis have made it clear that each brain malformation is phenotypically "unique" and causally heterogeneous. Molecular studies have shown that mutations in different genes involved in a signaling pathway may result in a similar malformation. In addition, signaling pathways may be a possible target of toxic agents, which will mimic the genetic causes of malformations. These findings have raised growing interest in the early patterning of the developing nervous system in humans and its molecular controlling pathways. Consequently, brain malformations are now evaluated with special regard to their mechanism and cause analysis, considering fetal, maternal, and placental pathology. The predictive value of this multidisciplinary approach is now well demonstrated and has led, in some conditions, to gene identification, which is crucial for genetic counseling. It permits a prenatal molecular diagnosis as early as the 10–12th gestational week on chorionic villus sampling.
Similar content being viewed by others
References
Ahdab-Barmada M, Classen D (1990) A distinctive triad of malformations of the central nervous system in the Meckel-Gruber syndrome. J Neuropathol Exp Neurol 49:610–620
Caspi M, Atlas R, Kantor A, Sapir T, Reiner O (2000) Interaction between LIS1 and doublecortin, two lissencephaly gene products. Hum Mol Genet 9:2205–2213
Cohen MM Jr, Sulik KK (1992) Perspectives on holoprosencephaly. II. Central nervous system, craniofacial anatomy, syndrome commentary, diagnostic approach, and experimental studies. J Craniofacial Genet Dev Biol 12:196–244
Cormand B, Pihko H, Bayes M, Valanne L, Santavuori P, Talim B, Gershoni-Baruch R, Ahmad A, van Bokhoven H, Brunner HG, Voit T, Topaloglu H, Dobyns WB, Lehesjoki AE (2001) Clinical and genetic distinction between Walker-Warburg syndrome and muscle-eye-brain disease. Neurology 56:1059–1069
Cortez SC, Kinney HC (1996) Brainstem tegmental necrosis and olivary hypoplasia: a lethal entity associated with congenital apnea. J Neuropathol Exp Neurol 55:841–849
De France I, Saada P, Jouannic JM, Tantau J, Martinovic J, Encha-Razavi F (2002) Ultrasonographic and pathological correlation in a fetal intracranial cyst: a case of "diencephalo-synapsis" J Gynecol Obstet Biol Reprod (Paris) 31:600–603
De Grouchy J, Turleau C (1984) Clinical atlas of human chromosomes, 2nd edn. Wiley, New York
Dobyns WB, Stratton RF, Greenberg F (1984) Syndromes with lissencephaly. I. Miller-Dieker and Norman-Roberts syndromes and isolated lissencephaly. Am J Med Genet 18:509–526
Dobyns WB, Kirkpatrick JB, Hittner HM, Roberts RM, Kretzer FL (1985) Syndromes with lissencephaly. II. Walker-Warburg and cerebro-oculo-muscular syndromes and a new syndrome with type II lissencephaly. Am J Med Genet 22:157–195
Dobyns WB, Gilbert EF, Opitz JM (1985) Further comments on the lissencephaly syndromes. Am J Med Genet 22:197–211
Dobyns WB, Truwit CL, Ross ME, Matsumoto N, Pilz DT, Ledbetter DH, Gleeson JG, Walsh CA, Barkovich AJ (1999) Differences in the gyral pattern distinguish chromosome 17-linked and X-linked lissencephaly. Neurology 53:270–277
Encha-Razavi F (1995) Fetal neuropathology. In: Duckett S (ed) Pediatric neuropathology. Williams and Wilkins, Baltimore, pp 108–122
Encha-Razavi F, Larroche JC, Roume J, Gonzales M, Kondo HC, Mulliez N (1996) Lethal familial fetal akinesia sequence (FAS) with distinct neuropathological pattern: type III lissencephaly syndrome. Am J Med Genet 62:16–22
Friede RL (1989) Developmental neuropathology, 2nd edn. Springer, Berlin Heidelberg New York
Golden JA (1998) Holoprosencephaly: a defect in brain patterning. J Neuropathol Exp Neurol 57:991–999
Guihard-Costa AM, Larroche JC (1995) Fetal biometry. Fetal Diagn Ther 10:211–276
Hall JG, Pallister PD, Clarren SK, Beckwith JB, Wiglesworth FW, Fraser FC, Cho S, Benke PJ, Reed SD (1980) Congenital hypothalamic hamartoblastoma, hypopituitarism, imperforate anus, and postaxial polydactyly—a new syndrome? I. Clinical, causal, and pathogenetic considerations. Am J Med Genet 7:47–74
Harper C (1998) The neuropathology of alcohol-specific brain damage, or does alcohol damage the brain? J Neuropathol Exp Neurol 57:101–110
Mahieu-Caputo D, Salomon LJ, Dommergues M, Aubry MC, Sonigo P, Martinovic Y, Le Merrer M, Dumez Y, Encha-Razavi F (2002) Arthrogryposis multiplex congenital and cerebellopontine ischemic lesions in sibs: recurrence of prenatal disruptive brain lesions with different patterns of expression? Fetal Diagn Ther 17:153–156
McMahon CL, Braddock SR (2001) Septo-optic dysplasia as a manifestation of valproic acid embryopathy. Teratology 64:83–86
Michaud J, Mizrahi EM, Urich H (1982) Agenesis of the vermis with fusion of the cerebellar hemispheres, septo-optic dysplasia and associated anomalies. Report of a case. Acta Neuropathol (Berl) 56:161–166
Muenke M, Beachy PH (2000) Genetics of ventral forebrain development and holoprosencephaly. Curr Opin Genet Dev 10:262–269
Norman MG, McGillivray BC, Kalousek DK, Hill A, Poskitt KJ (1995) Congenital malformations of the brain. Pathological, embryological, radiological and genetic aspects. Oxford University Press, New York
Pilz D, Stoodley N, Golden JA (2002) Neuronal migration, cerebral cortical development and cerebral cortical anomalies. J Neuropathol Exp Neurol 61:1–11
Van Camp G, Frasen E, Vits L, Raes G, Willems PJ (1996) A locus-specific mutation database for the neural cell adhesion molecule L1CAM (Xq28). Hum Mutat 8:391
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Encha-Razavi, F. Identification of brain malformations: neuropathological approach. Childs Nerv Syst 19, 448–454 (2003). https://doi.org/10.1007/s00381-003-0764-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-003-0764-7