Abstract
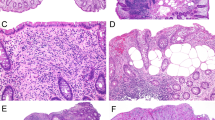
The hamartomatous polyposis syndromes are a heterogeneous group of disorders that share an autosomal-dominant pattern of inheritance and are characterized by hamartomatous polyps of the gastrointestinal tract. These syndromes include juvenile polyposis syndrome, Peutz–Jeghers syndrome and the PTEN hamartoma tumor syndrome. The frequency and location of the polyps vary considerably among syndromes, as does the affected patient's predisposition to the development of gastrointestinal and other malignancies. Although the syndromes are uncommon, it is important for the clinician to recognize these disorders because they are associated with considerable morbidity and mortality, not only from malignancy but also from nonmalignant manifestations such as bleeding, intussusception, and bowel obstruction. Each hamartomatous polyposis syndrome has its own distinctive organ-specific manifestations and each requires a different surveillance strategy, which makes accurate diagnosis crucial for appropriate patient management. The availability of clinical genetic testing for these disorders means that appropriate recognition allows for timely referral for cancer genetic counseling, and often allows for predicative testing in at-risk family members. Promisingly, an understanding of the molecular pathogenesis of these disorders offers insights into the mechanisms underlying the development of sporadic malignancy, and enables rational selection of targeted therapies that warrant further investigation.
Key Points
-
Hamartomatous polyposis syndromes are inherited autosomal-dominant syndromes that confer predisposition to cancers and have divergent clinical features, but often involve interconnected molecular pathways
-
Juvenile polyposis syndrome is caused by germline mutations of SMAD4, BMPR1A and ENG, and it predisposes individuals to colon cancer, and, to a lesser extent, upper gastrointestinal malignancies
-
Cowden syndrome, the most common PTEN hamartoma tumor syndrome, is caused by germline PTEN mutations and is characterized by benign and malignant breast, thyroid and endometrial manifestations, in addition to macrocephaly and characteristic mucocutaneous findings
-
Peutz–Jeghers syndrome is caused by germline STK11 mutations and is associated with a markedly increased risk of gastrointestinal, breast and gynecologic malignancies
-
Timely diagnosis of hamartomatous polyposis syndromes allows for appropriate surveillance and management, which varies considerably between syndromes
-
Clinical testing for germline mutations should occur in the setting of appropriate genetic counseling and offer predictive testing for family members
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Nagy R et al. (2004) Highly penetrant hereditary cancer syndromes. Oncogene 23: 6445–6470
Wang ZJ et al. (1999) Allelic imbalance at the LKB1 (STK11) locus in tumours from patients with Peutz–Jeghers' syndrome provides evidence for a hamartoma-(adenoma)-carcinoma sequence. J Pathol 188: 9–13
Kutscher AH et al. (1960) Incidence of Peutz–Jeghers syndrome. Am J Dig Dis 5: 576–577
Utsunomiya J et al. (1975) Peutz–Jeghers syndrome: its natural course and management. Johns Hopkins Med J 136: 71–82
McGarrity TJ and Amos C (2006) Peutz–Jeghers syndrome: clinicopathology and molecular alterations. Cell Mol Life Sci 63: 2135–2144
Giardiello FM and Trimbath JD (2006) Peutz–Jeghers syndrome and management recommendations. Clin Gastroenterol Hepatol 4: 408–415
Giardiello FM et al. (1987) Increased risk of cancer in the Peutz–Jeghers syndrome. N Engl J Med 316: 1511–1514
Estrada R and Spjut HJ (1983) Hamartomatous polyps in Peutz–Jeghers syndrome. A light-, histochemical, and electron-microscopic study. Am J Surg Pathol 7: 747–754
Giardiello FM et al. (2000) Very high risk of cancer in familial Peutz–Jeghers syndrome. Gastroenterology 119: 1447–1453
Lim W et al. (2004) Relative frequency and morphology of cancers in STK11 mutation carriers. Gastroenterology 126: 1788–1794
Srivatsa PJ et al. (1994) Disseminated cervical adenoma malignum and bilateral ovarian sex cord tumors with annular tubules associated with Peutz–Jeghers syndrome. Gynecol Oncol 53: 256–264
Scully RE et al. (1970) Sex cord tumor with annular tubules a distinctive ovarian tumor of the Peutz–Jeghers syndrome. Cancer 25: 1107–1121
Terauchi S et al. (2006) Double-balloon endoscopy and Peutz–Jeghers syndrome: a new look at an old disease. Proc (Bayl Univ Med Cent) 19: 335–337
Volikos E et al. (2006) LKB1 exonic and whole gene deletions are a common cause of Peutz–Jeghers syndrome. J Med Genet 43: e18
Sweet K et al. (2005) Molecular classification of patients with unexplained hamartomatous and hyperplastic polyposis. JAMA 294: 2465–2473
Alessi DR et al. (2006) LKB1-dependent signaling pathways. Annu Rev Biochem 75: 137–163
Corradetti MN et al. (2004) Regulation of the TSC pathway by LKB1: evidence of a molecular link between tuberous sclerosis complex and Peutz–Jeghers syndrome. Genes Dev 18: 1533–1538
Amos CI et al. (2004) Genotype-phenotype correlations in Peutz–Jeghers syndrome. J Med Genet 41: 327–333
Miyoshi H et al. (2002) Gastrointestinal hamartomatous polyposis in Lkb1 heterozygous knockout mice. Cancer Res 62: 2261–2266
Zbuk KM and Eng C (2007) Cancer phenomics: RET and PTEN as illustrative models. Nat Rev Cancer 7: 35–45
Nelen MR et al. (1997) Germline mutations in the PTEN/MMAC1 gene in patients with Cowden disease. Hum Mol Genet 6: 1383–1387
The NCCN Genetic/Familial High-Risk Assessment: Breast and Ovarian Guideline (V.1.2007) © 2006 National Comprehensive Cancer Network, Inc. To view the most recent and complete version of the guideline, go online to www.nccn.org (accessed July 1 2007)
Gorlin RJ et al. (1992) Bannayan–Riley–Ruvalcaba syndrome. Am J Med Genet 44: 307–314
Wiedemann HR et al. (1983) The proteus syndrome. Partial gigantism of the hands and/or feet, nevi, hemihypertrophy, subcutaneous tumors, macrocephaly or other skull anomalies and possible accelerated growth and visceral affections. Eur J Pediatr 140: 5–12
Starink TM et al. (1986) The Cowden syndrome: a clinical and genetic study in 21 patients. Clin Genet 29: 222–233
Weber HC et al. (1998) Germline PTEN/MMAC1/TEP1 mutations and association with gastrointestinal manifestations in Cowden disease. Gastroenterology 114: 2902
Marra G et al. (1994) Cowden's disease with extensive gastrointestinal polyposis. J Clin Gastroenterol 18: 42–47
McGarrity TJ et al. (2003) GI polyposis and glycogenic acanthosis of the esophagus associated with PTEN mutation positive Cowden syndrome in the absence of cutaneous manifestations. Am J Gastroenterol 98: 1429–1434
Eng C (2000) Will the real Cowden syndrome please stand up: revised diagnostic criteria. J Med Genet 37: 828–830
Marsh DJ et al. (1998) Mutation spectrum and genotype-phenotype analyses in Cowden disease and Bannayan-Zonana syndrome, two hamartoma syndromes with germline PTEN mutation. Hum Mol Genet 7: 507–515
Bosserhoff AK et al. (2006) Multiple colon carcinomas in a patient with Cowden syndrome. Int J Mol Med 18: 643–647
Carethers JM et al. (1998) Absence of PTEN/MMAC1 germ-line mutations in sporadic Bannayan–Riley–Ruvalcaba syndrome. Cancer Res 58: 2724–2726
Zigman AF et al. (1997) Localization of the Bannayan–Riley–Ruvalcaba syndrome gene to chromosome 10q23. Gastroenterology 113: 1433–1437
Zhou XP et al. (2003) Germline PTEN promoter mutations and deletions in Cowden/Bannayan–Riley–Ruvalcaba syndrome result in aberrant PTEN protein and dysregulation of the phosphoinositol-3-kinase/Akt pathway. Am J Hum Genet 73: 404–411
Suzuki A et al. (1998) High cancer susceptibility and embryonic lethality associated with mutation of the PTEN tumor suppressor gene in mice. Curr Biol 8: 1169–1178
Waite KA and Eng C (2002) Protean PTEN: form and function. Am J Hum Genet 70: 829–844
Chow LM and Baker SJ (2006) PTEN function in normal and neoplastic growth. Cancer Lett 241: 184–196
Di Cristofano A et al. (1998) Pten is essential for embryonic development and tumour suppression. Nat Genet 19: 348–355
Toccalino H et al. (1973) Juvenile polyps of the rectum and colon. Acta Paediatr Scand 62: 337–340
Doxey BW et al. (2005) Inherited polyposis syndromes: molecular mechanisms, clinicopathology, and genetic testing. Clin Gastroenterol Hepatol 3: 633–641
Jass JR et al. (1988) Juvenile polyposis—a precancerous condition. Histopathology 13: 619–630
Giardiello FM et al. (1991) Colorectal neoplasia in juvenile polyposis or juvenile polyps. Arch Dis Child 66: 971–975
Howe JR et al. (1998) The risk of gastrointestinal carcinoma in familial juvenile polyposis. Ann Surg Oncol 5: 751–756
Sayed MG et al. (2002) Germline SMAD4 or BMPR1A mutations and phenotype of juvenile polyposis. Ann Surg Oncol 9: 901–906
Friedl W et al. (2002) Juvenile polyposis: massive gastric polyposis is more common in MADH4 mutation carriers than in BMPR1A mutation carriers. Hum Genet 111: 108–111
Coburn MC et al. (1995) Malignant potential in intestinal juvenile polyposis syndromes. Ann Surg Oncol 2: 386–391
Schreibman IR et al. (2005) The hamartomatous polyposis syndromes: a clinical and molecular review. Am J Gastroenterol 100: 476–490
Brosens LA et al. (2007) Risk of colorectal cancer in juvenile polyposis. Gut 56: 965–967
Cao X et al. (2006) Mapping of hereditary mixed polyposis syndrome (HMPS) to chromosome 10q23 by genomewide high-density single nucleotide polymorphism (SNP) scan and identification of BMPR1A loss of function. J Med Genet 43: e13
Gallione CJ et al. (2004) A combined syndrome of juvenile polyposis and hereditary haemorrhagic telangiectasia associated with mutations in MADH4 (SMAD4). Lancet 363: 852–859
Waite KA and Eng C (2003) From developmental disorder to heritable cancer: it's all in the BMP/TGF-beta family. Nat Rev Genet 4: 763–773
Wang J et al. (1995) Demonstration that mutation of the type II transforming growth factor beta receptor inactivates its tumor suppressor activity in replication error-positive colon carcinoma cells. J Biol Chem 270: 22044–22049
Grady WM et al. (1999) Mutational inactivation of transforming growth factor beta receptor type II in microsatellite stable colon cancers. Cancer Res 59: 320–324
Grady WM and Markowitz SD (2002) Genetic and epigenetic alterations in colon cancer. Annu Rev Genomics Hum Genet 3: 101–128
Howe JR et al. (2004) The prevalence of MADH4 and BMPR1A mutations in juvenile polyposis and absence of BMPR2, BMPR1B, and ACVR1 mutations. J Med Genet 41: 484–491
Howe J et al. (2007) ENG mutations in MADH4/BMPR1A mutation negative patients with juvenile polyposis. Clin Genet 71: 91–92
Delnatte C et al. (2006) Contiguous gene deletion within chromosome arm 10q is associated with juvenile polyposis of infancy, reflecting cooperation between the BMPR1A and PTEN tumor-suppressor genes. Am J Hum Genet 78: 1066–1074
Tsuchiya KD et al. (1998) Deletion 10q23.2-q23.33 in a patient with gastrointestinal juvenile polyposis and other features of a Cowden-like syndrome. Genes Chromosomes Cancer 21: 113–118
Jacoby RF et al. (1997) Del(10)(q22.3q24.1) associated with juvenile polyposis. Am J Med Genet 70: 361–364
Eng C and Ji H (1998) Molecular classification of the inherited hamartoma polyposis syndromes: clearing the muddied waters. Am J Hum Genet 62: 1020–1022
Eng C (2001) To be or not to BMP. Nat Genet 28: 105–107
Takaku K et al. (1999) Gastric and duodenal polyps in Smad4 (Dpc4) knockout mice. Cancer Res 59: 6113–6117
Mishina Y et al. (1995) Bmpr encodes a type I bone morphogenetic protein receptor that is essential for gastrulation during mouse embryogenesis. Genes Dev 9: 3027–3037
Bourdeau A et al. (1999) A murine model of hereditary hemorrhagic telangiectasia. J Clin Invest 104: 1343–1351
Chan OT and Haghighi P (2006) Hamartomatous polyps of the colon: ganglioneuromatous, stromal, and lipomatous. Arch Pathol Lab Med 130: 1561–1566
Jacob S et al. (1998) Neurofibromatosis of the colon: an unusual manifestation of von Recklinghausen's diseases—a case report. Indian J Pathol Microbiol 41: 113–116
Schwartz RA (1978) Basal-cell-nevus syndrome and gastrointestinal polyposis. N Engl J Med 299 49
Whitelaw SC et al. (1997) Clinical and molecular features of the hereditary mixed polyposis syndrome. Gastroenterology 112: 327–334
Jaeger EE et al. (2003) An ancestral Ashkenazi haplotype at the HMPS/CRAC1 locus on 15q13-q14 is associated with hereditary mixed polyposis syndrome. Am J Hum Genet 72: 1261–1267
Fran DN et al. (2006) Rapamycin causes regression of astrocytomas in tuberous sclerosis complex. Ann Neurol 59: 490–498
Rubio-Viqueira B and Hidalgo M (2006) Targeting mTOR for cancer treatment. Adv Exp Med Biol 587: 309–327
Udd L et al. (2004) Suppression of Peutz–Jeghers polyposis by inhibition of cyclooxygenase-2. Gastroenterology 127: 1030–1037
Brazowski E et al. (2005) Characteristics of familial juvenile polyps expressing cyclooxygenase-2. Am J Gastroenterol 100: 130–138
Bosman FT (1999) The hamartoma-adenoma-carcinoma sequence. J Pathol 188: 1–2
Perzin KH and Bridge MF (1982) Adenomatous and carcinomatous changes in hamartomatous polyps of the small intestine (Peutz–Jeghers syndrome): report of a case and review of the literature. Cancer 49: 971–983
Mills SE and Fechner RE (1982) Unusual adenomatous polyps in juvenile polyposis coli. Am J Surg Pathol 6: 177–183
Jansen M et al. (2006) Mucosal prolapse in the pathogenesis of Peutz–Jeghers polyposis. Gut 55: 1–5
Clevers H (2005) Stem cells, asymmetric division and cancer. Nat Genet 37: 1027–1028
Bronner M (2003) Gastrointestinal inherited polyposis syndromes. Mod Path 16: 359–365
Acknowledgements
KM Zbuk is a Crile Fellow of the Cleveland Clinic, USA. C Eng is a recipient of the Doris Duke Distinguished Clinical Scientist Award and is supported by grants from the US National Institutes of Health, US National Cancer Institute and the American Cancer Society. Désirée Lie, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the Medscapeaccredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Zbuk, K., Eng, C. Hamartomatous polyposis syndromes. Nat Rev Gastroenterol Hepatol 4, 492–502 (2007). https://doi.org/10.1038/ncpgasthep0902
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpgasthep0902
This article is cited by
-
SMAD4 variants and its genotype–phenotype correlations to juvenile polyposis syndrome
Hereditary Cancer in Clinical Practice (2023)
-
Characteristics and potential malignancy of colorectal juvenile polyps in adults: a single-center retrospective study in China
BMC Gastroenterology (2022)
-
Considerations on diagnosis and surveillance measures of PTEN hamartoma tumor syndrome: clinical and genetic study in a series of Spanish patients
Orphanet Journal of Rare Diseases (2022)
-
Endoscopic Management of Hamartomatous Polyposis Syndromes
Current Treatment Options in Gastroenterology (2021)
-
Peutz-Jeghers Syndrome Presented as Jejunojejunal Intussusception
Indian Journal of Surgery (2021)