Abstract
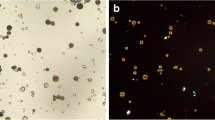
Although gout and hyperuricaemia are usually thought of as conditions of indulgent male middle age, in addition to the well-known uricosuria of the newborn, there is much of importance for the paediatric nephrologist in this field. Children and infants may present chronically with stones or acutely with renal failure from crystal nephropathy, as a result of inherited deficiencies of the purine salvage enzymes hypoxanthine-guanine phosphoribosyltransferase (HPRT) and adenine phosphoribosyltransferase (APRT) or of the catabolic enzyme xanthine dehydrogenase (XDH). Genetic purine overproduction in phosphoribosylpyrophosphate synthetase superactivity, or secondary to glycogen storage disease, can also present in infancy with renal complications. Children with APRT deficiency may be difficult to distinguish from those with HPRT deficiency because the insoluble product excreted, 2,8-dihydroxyadenine (2,8-DHA), is chemically very similar to uric acid. Moreover, because of the high uric acid clearance prior to puberty, hyperuricosuria rather than hyperuricaemia may provide the only clue to purine overproduction in childbood. Hyperuricaemic renal failure may be seen also in treated childhood leukaemia and lymphoma, and iatrogenic xanthine nephropathy is a potential complication of allopurinol therapy in these conditions. The latter is also an under-recognised complication of treatment in the Lesch-Nyhan syndrome or partial HPRT deficiency. The possibility of renal complications in these three situations is enhanced by infection, the use of uricosuric antibiotics and dehydration consequent upon fever, vomiting or diarrhoea. Disorders of urate transport in the renal tubule may also present in childhood. A kindred with X-linked hereditary nephrolithiasis, renal urate wasting and renal failure has been identified, but in general, the various rare types of net tubular wasting of urate into the urine are recessive and relatively benign, being found incidentally or presenting as colic from crystalluria. However, the opposite condition of a dominantly inherited increase in net urate reabsorption is far from benign, presenting as familial renal failure, with hyperuricaemia either preceding renal dysfunction or disproportionate to it. Paediatricians need to be aware of the lower plasma urate concentrations in children compared with adults when assessing plasma urate concentrations in childhood and infancy, so that early hyperuricosuria is not missed. This is of importance because most of the conditions mentioned above can be treated successfully using carefully controlled doses of allopurinol or means to render urate more soluble in the urine. Xanthine and 2,8-DHA are extremely insoluble at any pH. Whilst 2,8-DHA formation can also be controlled by allopurinol, alkali is contraindicated. A high fluid, low purine intake is the only possible therapy for XDH deficiency.
Similar content being viewed by others
References
Kelley WN, Wyngaarden JM (1976) Gout and hyperuricemia. Grune and Stratton, New York
Scriver CR, Beaudet AL, Sly S, Valle D (eds) (1989) The metabolic basis of inherited disease, 6th edn, McGraw-Hill, New York
Stone TW, Simmonds HA (1991) Purines: basic and clinical aspects, Kluwer, London
Cameron JS, Simmonds HA (1981) Uric acid, gout and the kidney. J Clin Pathol 34: 1245–1254
Simmonds HA, Van Acker KJ, Cameron JS, Snedden W (1976) The identification of 2,8-dihydroxyadenine, a new component of urinary stones. Biochem J 157: 485–487
Colussi G, Rambola G, Ferrari ME de, Rolando P, Surian M, Malberti F, Minetti L (1987) Pharmacological evaluation of urate handling in humans: pyrazinamide test vs combined pyrazinamide and probenecid administration. Nephrol Dial Transplant 2: 10–16
Diamond HS (1989) Interpretation of pharmacologic manipulation of urate transport in man. Nephron 51: 1–5
Sanchez Bayle M, Vasquez Martul M, Ecija Peiro JL, Garcia Vao C, Ramo Mancheno C (1987) Renal handling of uric acid in normal children by means of pyrazinamide and sulfinpyrazone tests. Int J Pediatr Nephrol 8: 5–8
Guggino SE, Aronson PS (1985) Paradoxical effects of pyrazinoate and nicotinate on urate transport in dog renal microvillus membranes. J Clin Invest 76: 543–547
Zöllner N, Gresser U (eds) (1991) Urate deposition in man and its clinical consequences. Springer, Berlin Heidelberg New York
Danovich GM, Weinberger J, Berlyne GM (1972) Uric acid in advanced renal failure. Clin Sci 43: 331–341
Boumendil-Podevin EF, Podevin RA, Richet G (1975) Uricosuric agents in uremic sera. Identification of indoxyl sulfate and hippuric acid. J Clin Invest 55: 1142–1152
Calabrese G, Simmonds HA, Cameron JS, Davies PM (1990) Precocious familial gout with reduced fractional excretion of urate and normal purine enzymes. Q J Med 75: 441–450
Cameron JS, Moro F, Simmonds HA (1991) What is the pathogenesis of familial juvenile gouty nephropathy? Adv Exp Med Biol 309 A: 185–191
Stapleton FB (1992) Uric acid nephropathy. In: Edelmann CE, et al (eds) Pediatric nephrology, 2nd edn. Little Brown, Boston, pp 1647–1659
Simmonds HA, Stutchbury JH, Webster DR, Spencer RE, Fisher RA, Wooder M, Buckley BM (1984) Pregnancy in xanthinuria: demonstration of fetal uric acid production? J Inherited Metab Dis 7: 77–79
Sanchez Bayle M, Martinez Jiminez AL, Ruiz-Jarabo C, Asensio J, Arniaz P, Vilay J, Baeza S (1992) Uricosuria en la infancia y adolescencia. Nefrología 12: 239–243
Sperling O (1989) Hereditary renal hypouricaemia. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic basis of inherited disease, 6th edn McGraw Hill, New York, pp 2605–2619
Simmonds HA, Duley JA, Davies PM (1991) Analysis of purines and pyrimidines in blood, urine and other physiological fluids. In: Hommes F (ed) Techniques in diagnostic human biochemical genetics. A Laboratory manual. Wiley. New York, pp 397–425
Wortman RL, Fox IH (1980) Limited value of uric acid to creatinine ratios in estimating uric acid excretion. Ann Intern Med 93: 822–827
Simmonds HA, Cameron JS, Barratt TM, Dillon MJ, Meadow SR, Trompeter RS (1989) Purine enzyme defects as a cause of acute renal failure in childhood. Pediatr Nephrol 3: 433–437
Cameron JS, Simmonds HA, Webster DR, Wass V, Sahota AS (1984) Problems of diagnosis in an adolescent with hypoxanthineguanine phosphoribosyltransferase deficiency. Adv Exp Med Biol 165A: 7–13
Page T, Nyhan WL (1989) The spectrum of HPRT deficiency: an update. Adv Exp Med Biol 253 A: 129–133
Watts RWE (1985) Defects of tetrahydrobiopterin synthesis and their possible relationship to a disorder of purine metabolism, the Lesch-Nyhan syndrome. Adv Enzyme Regul 23: 25–58
Davidson BL, Tarle SA, Van Antwerp M, Gibbs DA, Watts RWE, Kelley WN, Palella TD (1991) Identification of 17 independent mutations responsible for human hypoxanthine-guanine phosphoribosyltransferase (HPRT) deficiency. Am J Hum Genet 48: 951–955
Mc Carthy G (1992) Practical aspect of the management of the Lesch-Nyhan syndrome. BIMDG Newsletter (in press)
Brock WA, Golden J, Kaplan GW (1983) Xanthine calculi in the Lesch Nyhan dyndrome. J Urol 130: 157–159
Kenney IJ (1991) Renal sonography in long standing Lesch Nyhan syndrome. Clin Radiol 43: 39–41
Simmonds HA, Cameron JS, Morris GS, Davies PM (1986) Allopurinol in renal failure and the tumour lysis syndrome. Clin Chim Acta 160: 189–195
Zoref E, Vries A de, Sperlin O (1975) Mutant feedback resistant phosphoribosylpyrophosphate synthetase associated with purine overproduction and gout. J Clin Invest 56: 1093–1099
Ishizuka T, Iizasa T, Taira M, Ishijima S, Sonodo T, Shimada H, Nagatake N, Tatibana M (1992) Promoter regions of the human X-linked housekeeping genes PRPS1 and PRPS2 encoding phophoribosylpyrphosphate synthetase subunit I and II. Biochim Biophys Acta 1130: 139–148
Roessler BJ, Golovoy N, Palella TD, Heidler S, Becker MA (1991) Identification of distinct PRS1 mutations in two patients with X-linked phosphoribosylpyrophosphate synthetase superactivity. Adv Exp Med Biol 309 B: 125–128
Ceballos-Picot I, Perignon JL, Hamet M, Daudon M, Kamoun P, (1992) 2,8-Dihydroxyadenine urolithiasis, an underdiagnosed disease. Lancet 339: 1050–1051
Kamatani N, Hakoda M, Otsuka S, Yoshikawa H, Kashiwazaki S (1992) Only three mutations account for almost all defective alleles causing adenine phosphoribosyltransferase deficiency in Japanese patients. J Clin Invest (in press)
Simmonds HA, Van Acker KJ, Sahota AS (1992) 2,8-Dihydroxyadenine lithiasis. Lancet 339: 1295–1296
Greenwood MC, Dillon MJ, Simmonds HA, Barratt TM, Pincott JR, Metreweli C (1982) Renal failure due to 2,8-dihydroxyadenine urolithiasis. Eur J Pediatr 138: 346–349
Chen J, Sahota A, Laxdal T, Scrine M, Bowmans Cui C, Stambrook PJ, Tischfield JA (1991) Identification of a single missense mutation in the adenine phosphoribosyltransferase gene from five Icelandic patients and a British patient. Am J Hum Genet 49: 251–254
Simmonds HA, Reiter S, Nishino T (1993) Hereditary xanthinuria. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic basis of inherited disease, 7th edn, McGraw Hill. New York (in press)
Dent CE, Philpot GR (1954) Xanthinuria, an inborn error (or deviation) of metabolism. Lancet I: 182–185
Carpenter TO, Lebowitz RL, Nelson D, Bauer S (1986) Hereditary xanthinuria presenting in infancy with nephrolithiasis. J Pediatr 109:307–309
Fildes RD (1989) Hereditary xanthinuria with severe urolithiasis occurring in infancy as renal tubular acidosis and hypercalciuria. J Pediant 115:277–208
Henderson MJ, Bradbury M, Brocklebank JT, Simmonds HA (1992) xanthinuria: presentation with acute renal failure in a ninemonth-old girl. Inher Metab Dis 15:302
Reiter S, Simmonds HA, Zollner N, Braun SL, Knedel M (1990) Demonstration of a combined deficiency of xanthine oxidase and aldehyde oxidase in xanthinuric patients not forming oxypurinol. Clin Chim Acta 187:221–234
Hille R, Massey V (1985) Molybdenum-containing hydroxylases: xanthine oxidase, aldehyde oxidase and sulfite oxidase. In: Spiro TP (ed) Molybdenum enzymes. Academic Press, New York, pp 443–518
Wahl RC, Warner CK, Finnerty V, Rajagopalan KV (1982)Orosophila melanogaster ma-1 mutants are defective in the sulfuration of desulfo Mo hydroxylases. J Biol Chem 257:3958–3963
Beedham C (1987) Molybdenum hydroxylases: biological distribution and substrate-inhibitor specificity. Prog Med Chem 24:85–127
Hillebrand G, Reiter S (1991) Hypourikämie — ein differentialdiagnostisches Problem. Internist (Berlin) 32:226–229
Johnson JL, Wuebbens MM, Mandell R, Shih VE (1988) Molybdenum cofactor deficiency in a patient previously characterised as deficient in sulfite oxidase. Biochem Med Metab Biol 40:86–93
Maynard J, Benson P (1988) Herediatary xanthinuria in 2 Pakistani sisters: asymptomatic in one with β-thalassemia but causing xanthine stone, obstructive uropathy and hypertension in the other. J Urol 139:338–339
Ablin A, Stephens BG, Hirata T, Wilson K, Williams HE (1972) Nephropathy, xanthinuria, and orotic aciduria complicating Burkitt's lymphoma treated with chemotherapy and allopurinol. Metabolism 21:771–775
Gomez GA, Stutzman L, Ming Chu T (1978) Xanthine nephropathy during chemotherapy in deficiency of hypoxanthine-guanine phosphoribosyltransferase. Arch Intern Med 138:1017–1019
Farebrother DA, Hatfield P, Simmonds HA, Cameron JS, Jones AS, Cadenhead A (1975) Experimental crystal nephropathy (one year study in the pig) Clin Nephrol 4:243–250
Hisatome I, Igino K, Kotake M, Ishiko R, Saito M, Hasegawa J, Mashiba M, Nakamoto S (1989) Cause of persistent hypouricemia in outpatients. Nephron 51:13–16
De Vries A, Sperling O (1979) Inborn hypouricemia due to isolated renal tubular defect. Biomedicine 30:75–80
Praetorius E, Kirk JE (1950) Hypouricemia; with evidence for tubularelimination of uric acid J Lab Clin Med 35:865–868
Greene ML, Marcus R, Aurbach GD, Kazam ES, Seegmiller JE (1972) Hypouricemia due to isolated renal tubular defect. Dalmatian dog mutation in man. Am J Med 53:361–367
Sperling O, Boer P, Weinberger A, Vries A de (1974) Hypouricemia, hypercalciuria and decreased bone density; a hereditary syndrome. Ann Inter Med 80:482–487
Matsuda O, Shiigai T, Ito Y, Aonuma K, Taekuchi J (1982) A case of familial renal hypouricaemia associated with increased secretion of para-aminohippurate and idiopathic edema. Nephron 30:178–186
Akaoka I, Nishizawa T, Yano E, Kamatani N, Nishida Y, Sasaki S (1977) Renal urate secretion in five cases of hypouricemia with an isolated renal defect of urate transport. J Rheumatol 4:86–94
Garcia Puig J, Mateos F, Munoz A, Gaspar G, Lesmes A, Ramos I, Ortiz J (1983) Renal handling of uric acid in normal subjects by means of the pyrazinamide and probenecid tests. Nephron 35:183–186
Barrientos A, Perez Diaz V, Diaz Gonzales R, Rodicio JL (1979) Hypouricemia by defect in the tubular reabsorption. Arch Intern Med 139:787–789
Shichiri M, Iwamoto H, Shigai T (1987) Hypouricemia due to increased tubular urate secretion. Nephron 45:31–34
Kawachi M, Kono N, Kiyokawa H, Mineo I, Nakajima H, Shimizu T, Yorifuji S, Kuwajima M, Tarui S (1992) Decreased renal clearance of xanthine and hypoxanthine in a patient with renal hypouricemia. Nephron 61:428–431
Frymoyer PA, Scheinman SJ, Dunham PB, Jones DB, Hueber P, Schroeder ET (1991) X-linked recessive nephrolithiasis with renal failure. N Engl J Med 325:681–686
Mitnick PD, Beck L (1979) Hypouricemia and malignant neoplasm. Arch Intern Med 139:186–187
Mir MA, Delamore IW (1974) Hypouricemia and proximal renal tubular dysfunction in acute myeloid leukaemia. BMJ 3:775–777
Tykarski A (1988) Mechanism of hypouricemia in Hodgkin's disease. Isolated defect in post secretory reabsorption of uric acid. Nephron 50:217–219
Bennett J, Bond J, Singer I, Gottlieb A (1972) Hypouricemia in Hodgkin's disease. Ann Intern Med 76:751–756
Kay ME, Gottlieb AJ (1973) Hypoaricemia in Hodgkin's disease. Cancer 32:1508–1511
Berger L, Yü T-F (1975) Renal function in gout. IV. An analysis of 524 gouty subjects including long-term studies. Am J Med 59: 605–613
Duncan H, Dixon A StJ (1960) Gout, familial hyperuricaemia, and renal disease. Q J Med 29:127–136
Moro F, Ogg CS, Simmonds HA, Cameron JS, Chantler C, McBride MB, Duley JA, Davies PM (1991) Familial juvenile gouty nephropathy with renal urate hypoexcretion preceding renal disease. Clin Nephrol 35:263–269
Puig JG, Miranda ME, Mateos FA, Picazo ML, Lopez M, Ortiz J (1991) Familial nephropathy and gout: which comes first? Adv Exp Med Biol 309A:195–198
Rosenbloom FM, Kelley WN, Carr AA, Seegmiller JE (1967) Familial nephropathy and gout in a kindred (abstract). Clin Res 15:270
Treadwell BLJ (1971) Juvenile gout. Ann Rheum Dis 30:279–280
Van Goor W, Kooiker CJ, Dorhout Mees EJ (1971) An unusual form of renal disease associated with gout and hypertension. J Clin Pathol 24:354–359
Bennett RM, Chait A, Lewis B (1973) Familial hyperuricaemia and hypertriglyceridaemia. Ann Rheum Dis 32:497–500
Thompson GR, Weiss JJ, Goldman RT, Rigg GA (1978) Familial occurrence of hyperuricemia, gout and medullary cystic disease. Arch Intern Med 138:1615–1617
Fessel WJ (1979) Renal outcomes of gout and hyperuricemia. Am J Med 67:74–82
Simmonds HA, Warren DJ, Cameron JS, Potter CF, Farebrother DA (1980) Familial gout and renal failure in young women Clin Nephrol 14:176–182
Simmonds HA, Cameron JS, Potter CF, Warren D, Gibson T, Farebrother D (1980) Renal failure in young subjects with familial gout. Adv Exp Med Biol 122A:15–20
Massari PU, Hsu CH, Barnes RV, Fox IH, Gikas PW, Weller JM (1980) Familial hyperuricemia and renal disease. Arch Intern Med 140:680–684
Richmond JM, Kincaid-Smith P, Whitworth JA, Becker GJ (1981) Familial urate nephropathy. Clin Nephrol 16:163–168
Hollingworth P, Scott JT (1983) Familial gout, hyperuricemia and renal impairment. Ann Rheum Dis 42 [Suppl 1]:87–88
Leumann EP, Wegmann W (1983) Familial nephropathy with hyperuricemia and gout. Nephron 34:51–57
Yarom A, Rennebohm RM, Strife F, Levinson JE (1984) Juvenile gouty arthritis. Am J Dis Child 138:955–957
Foreman JW, Yudkoff M (1990) Familial hyperuricemia and renal insufficiency. Child Nephrol Urol 10:115–118
Mukarami T, Kawakami H, Nakatsuda K, Jojima K, Nohno H, Matsuzaki H (1990) Underexcretory-type hyperuricemia, disproportionate to the reduced glomerular filtration rate, in two boys with mild proteinuria. Nephron 56:439–442
McBride MB, Raman V, Ogg CS, Chantler C, Cameron JS, Duley J, Simmonds HA (1991) A new kindred with familial juvenile gouty nephropathy Adv Exp Med Biol 309A:191–194
Yokota N, Yamanaka H, Yamamoto Y, Fujimoto S, Eto T, Tanaka K (1991) Autosomal dominant transmission of gouty arthritis with renal disease in a large Japanese family. Ann Rheum Dis 50:108–111
Moro F, Simmonds HA, McBride MB, Cameron JS, Williams DG, Ogg CS (1991) Does allopurinol ameliorate progression in familial juvenile gouty nephropathy (FJGN)? Adv Exp Med Biol 309A: 199–202
Werner D, Martinez F, Roch-Ramel F (1990) Urate andp-aminohyppurate transport in the brush border membrane of the pig kidney. J Pharmacol Exp Ther 252:792–795
Werner D, Guisan B, Roch-Ramel F (1991) Urate transport in the proximal tubule of human kidney Adv Exp Med Biol 309A:177–180
Zmuda MJ, Quebbemann AJ (1975) Localisation of the renal tubular uric acid defect in gouty chickens Am J Physiol 229:820–825
Macdermot KD, Allsop J, Watts RWE (1984) The rate of purine synthesis de novo in blood mononuclear cells in vitro from patients with hyperuricaemic nephropathy. Clin Sci 67:249–258
Farebrother DA, Pincott JR, Simmonds HA, Warren DJ, Dillon MJ, Cameron JS (1981) Uric acid crystal-induced nephropahty: evidence for a specific renal lesion in a gouty family. J Pathol 135:159–168
Emmerson BT, Row G (1975) An evaluation of the pathogenesis of the gouty kidney. Kidney Int 8:65–71
Bennett WM (1985) Lead nephropathy. Kidney Int 28:212–220
Lin H-Y, Rocher LL, McQuillan MM, Schmaltz S, Palella TD, Fox IH (1989) Cyclosporine-induced hyperuricemia and gout N Engl J Med 321:287–292
Neilson EG, McCafferty E, Feldman A, Clayman MD, Zakheim B, Korngold R (1984) Spontaneous interstitial nephritis in kd.kd mice. I. A new model of autoimmune renal disease. J Immunol 133:2560–2565
Kelly CJ, Neilson EG (1987) Medullary cystic disease: an inherited form of autoimmune interstitial nephritis? Am J Kidney Dis 10:389–395
Palella T, Fox IH (1989) Hyperuricemia and gout. In: Scriver CR, Beaudet AL, Sly S, Valle D (eds) The metabolic basis of inherited disease, 6th edn McGraw-Hill, New York, pp 965–1007
Burke JR, Inglis JA, Craswell PW, et al (1982) Juvenile nephronophthisis and medullary cystic disease — the same disease (report of a large family with medullary cystic disease associated with gout and epilepsy). Clin Nephrol 18:1–8
Kleinknecht C, Habib R (1992) Nephronophthisis. In: Cameron JS, Davision AM, Grünfeld JP, Kerr DNS, Ritz E (eds) Oxford texbook of clinical nephrology. Oxford University Press, London, pp 2188–2197
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Cameron, J.S., Moro, F. & Simmonds, H.A. Gout, uric acid and purine metabolism in paediatric nephrology. Pediatr Nephrol 7, 105–118 (1993). https://doi.org/10.1007/BF00861588
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00861588